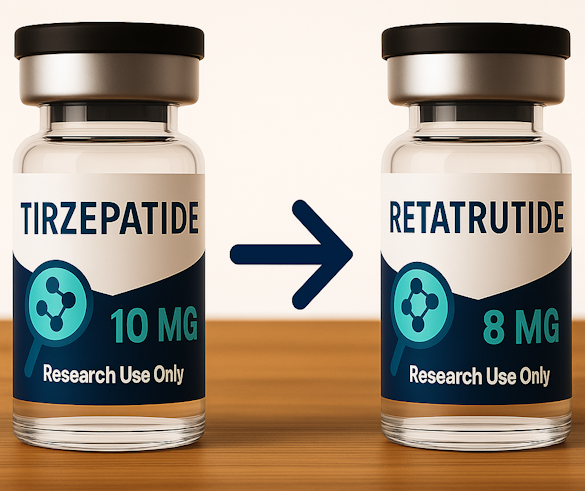
Maybe you’ve been on tirzepatide for a while, you’ve seen some results in your body weight, and now you’re hearing about retatrutide vs tirzepatide and thinking: Should I switch? How do I switch? Let’s walk through it together.
This article is going to guide you step-by-step through the process of switching from tirzepatide to retatrutide — what to know, how to prepare, how to communicate with your healthcare provider, and what to expect once you make the change.
For sourcing legitimate vials, start with our Where To Get Retatrutide Guide.
Why Consider Switching
There are a few practical reasons you might be thinking about switching from tirzepatide to retatrutide. First, tirzepatide is a dual agonist (targeting both GLP-1 and GIP receptors) and has proven results for weight loss and glycemic control. Retatrutide, on the other hand, is a newer investigational agent described as a triple-agonist (targeting GLP-1, GIP, and glucagon receptors) and has demonstrated promising early data for greater weight reduction and fat-burning potential.
So if you’re feeling like you’ve plateaued, your body weight isn’t moving as much as you hoped, or you want a next step in terms of what might help improve your metabolic health and weight management, switching could be a logical conversation.
That said — it’s not automatic or appropriate for everyone, especially when considering the differences between retatrutide and tirzepatide. Your individual response, your current regimen, side-effects, insurance/coverage, and most importantly, your healthcare provider’s input all matter.
When & How to Start the Transition
Here’s a practical outline for how someone might go about switching from tirzepatide to retatrutide — always under supervision of a healthcare provider.
1. Evaluate where you are on tirzepatide.
Before you consider the switch, check in on your current status: what dose you’re on, how well you’re tolerating it, what your body weight and metabolic markers (blood sugar, HbA1c, lipids) are doing, and whether you’re experiencing side-effects or plateauing. With tirzepatide, the usual starting dose is 2.5 mg once weekly, with increases every ~4 weeks if tolerated, up to a maintenance dose of 5-15 mg weekly for weight loss.
You might decide you’re ready for a change if you’ve been stable on tirzepatide for several months, are tolerating it well, but are no longer making meaningful progress in body weight or fat loss or metabolic health.
2. Talk to your healthcare provider about the “why” and “when.”
You and your provider will want to decide when to stop tirzepatide (or taper) and when to start retatrutide. Retatrutide isn’t yet fully FDA-approved for all settings (it’s still investigational in many uses) so this becomes a shared decision-making process.
You’ll want to review your blood sugar control (if you’re using tirzepatide partly for glycemic control), blood pressure, kidney/liver function, any GI side-effects, and your overall weight-loss journey.
3. Decide on a wash-out or direct switch?
In many cases, what happens is: finish your current cycle of tirzepatide (or reduce to a stable dose), then after a defined interval (often one week or so) begin retatrutide at the low dose under provider monitoring. Because retatrutide may have stronger effects or different side-effect profiles that could help reduce appetite, starting low is key.
Your healthcare provider might suggest you hold the last tirzepatide dose, wait seven days (or according to your specific regimen), then start retatrutide. Tapering or stopping tirzepatide may also help your body adjust and reduce overlapping side-effect risk.
4. Start retatrutide at a low dose and titrate.
Though exact dosing for retatrutide in the weight-loss setting is still being defined (because many of the uses remain investigational), in the key trial adults with obesity treated weekly showed large body weight reductions: e.g., up to ~17.5% at 24 weeks and up to ~24% at 48 weeks in certain dose groups.
Your provider may initiate retatrutide at the lowest available investigational dose, monitor your response (body weight, appetite, blood sugar, side-effects), then decide on dose escalation (“dose escalation”) as tolerated — similar in principle to how tirzepatide is titrated but potentially with more caution. Because retatrutide has shown more potent effects (and potentially more side-effects) you’ll want to proceed slowly under supervision.
5. Monitor labs and metrics.
While switching, you’ll want to track the progress towards achieving significant weight loss:
- body weight and waist circumference (to monitor fat loss and body composition)
- blood sugar / HbA1c / fasting insulin (for glycemic control)
- blood pressure and heart rate (some of these medications can raise heart-rate)
- side-effects: GI symptoms (nausea, vomiting), possible more intense responses with retatrutide
- your diet, hydration status, and workout/energy levels (as your body adjusts to the new medicine) Regular check-ins (every 4 weeks initially) help your provider catch anything needing adjustment.
Reference our Retatrutide Dosage Chart for aligning weekly dose equivalents.
What to Expect During the Switch
Switching from tirzepatide to retatrutide is a transition, and your body adjusts. Here’s what you might realistically expect:
- Because retatrutide has in trials produced greater weight loss than many earlier treatments (for example, in one study adults on the higher dose lost ~24% of their starting weight in ~48 weeks) you may see a faster drop in body weight and fat mass than you experienced on tirzepatide.
- With increased potency comes increased vigilance: GI side-effects may be more pronounced (nausea, slowed digestion, appetite suppression) so starting low and giving your body time is wise.
- Your appetite suppression may deepen and your energy expenditure (fat metabolism, fat loss) may improve — but that also means you’ll want to ensure you’re eating enough protein, maintaining lean mass, staying hydrated, and not inadvertently losing muscle mass.
- You may notice changes in how you respond to diet and exercise: for instance, less hunger, smaller portions, fewer cravings, and more rapid fat loss (especially if you pair it with your current healthy habits). But you’ll also want to listen to your body — if energy dips too much, or workouts feel drained, you might need to adjust your routine.
- Blood-sugar control and glycemic outcomes may still improve or continue improving (especially if you had diabetes or impaired glucose management) — retatrutide’s mechanism supports glucose control in addition to weight-loss.
- Because the transition is a change in your medication regimen, side-effects or unusual responses are possible: increased heart rate, more intense nausea, possibly more rapid drop in body weight requiring nutritional adjustments. Make sure your healthcare provider is aware of everything.
Practical Tips & Safety Considerations
Here are some friendly, real-world considerations as you make the switch:
- Keep your healthcare provider fully in the loop. This is key. Because retatrutide is still investigational in many uses and switching medications involves risk, you’ll want professional supervision rather than DIY.
- Plan your diet and activity accordingly. Even though the medication works, it doesn’t replace good habits. You’ll want to continue a reduced-calorie diet (as advised), regular physical activity, strength training to preserve lean muscle, and pay attention to your body composition (not just scale weight).
- Hydration and GI side-effect mitigation. If you experience nausea, vomiting, or slowed digestion (common with these medications), keep water and mild snacks handy, avoid large meals initially, and ask your clinician about supportive options (like anti-nausea strategies).
- Adjust your workout intensity if your body weight changes fast. If you’re losing body weight and fat rapidly, your energy may fluctuate; consider tweaking your HIIT or resistance training accordingly (less high stress if you’re feeling drained, more rest if needed).
- Monitor other health metrics. Aside from body weight and blood sugar, watch for heart-rate changes, blood pressure shifts (they may go down with weight loss, but your heart-rate might go up temporarily), and how your body adjusts to the new medication.
- Expect a period of adjustment. Switching medications often involves your body adjusting to a new “set-point”. You might feel more fatigue, changes in mood or food response, or different cravings in the first few weeks — that’s normal, and usually improves.
- Be realistic and patient. While retatrutide shows impressive results in early studies (e.g., significant body weight reductions), individual responses vary. It’s not just about the medication — your individual response, your lifestyle, your health status all matter.
- Consider cost and insurance coverage. Because retatrutide is investigational for many uses, insurance coverage might be limited. Make sure you understand the cost implications, and discuss with your clinician.
- Don’t stop tirzepatide cold turkey without guidance. If you’re already on tirzepatide and doing well, you don’t want to stop without a plan — abrupt stops may risk rebound appetite, glucose changes, or losing the momentum you built.
- Track progress comprehensively. Use tools: body weight log, waist circumference tape, progress in workouts, labs (HbA1c, fasting glucose, fasting insulin, lipid panel), side-effect log. That gives both you and your provider a clear picture.
Understand peptide sourcing concerns in Can You Trust Bulk Retatrutide From China?
Frequently Asked Questions
How do I start retatrutide?
Under your healthcare provider’s supervision, you’ll likely stop or taper down the tirzepatide dose, allow a short interval for your body to settle, then begin retatrutide at a low dose weekly. From there you’ll monitor appetite, body weight, blood sugar, side-effects, and your provider will determine when (and whether) to increase the dose to improve blood sugar control.
Is retatrutide stronger than tirzepatide?
In early studies, retatrutide has shown more pronounced weight loss and fat-burning potential compared to what many patients experience on tirzepatide or other dual-agonist medications. For example, in a 48-week trial, retatrutide induced body weight reductions of ~24% in some groups. That said, “stronger” also means different risk/monitoring profiles — so it’s not simply “better” for everyone.
How quickly does retatrutide work?
You may begin seeing changes in appetite suppression and possibly energy expenditure within the first few weeks of starting retatrutide, but significant body weight reduction tends to occur over months (24-48 weeks in trials show major changes). So, expect gradual change rather than overnight results.
How often can you take retatrutide?
In clinical trials, retatrutide has been administered once-weekly via subcutaneous injection. However, because it’s still investigational for broad weight-loss use, dosing frequency and long‐term schedule should be determined by a healthcare provider.
Follow proper mixing procedures using our Reconstitution Guide.
Conclusion
Switching from tirzepatide to retatrutide can absolutely make sense for some people — especially if you’ve done well on tirzepatide but feel ready for a next step in your weight-loss and metabolic-health journey. The key takeaways? It requires planning, communication with your healthcare provider, careful monitoring (of body weight, appetite, blood sugar, side-effects), and realistic expectations for sustained weight management. You may see deeper body weight and fat loss, improved glucose control, and intensified changes — but those gains come with increased need for supervision and support.
If you’re ready to upgrade your journey and your physician gives the green light, the switch from tirzepatide to retatrutide could be the next step to promote weight loss in your wellness story.
For comparative performance, review both Retatrutide vs Semaglutide and Mazdutide vs Retatrutide.